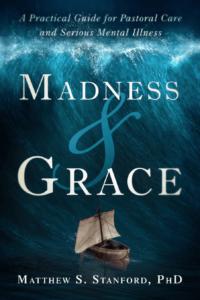
The church is the first place most individuals with mental illness seek help, even those with serious mental illness. Ann Michel interviews Dr. Matthew Stanford about his new book Madness and Grace: A Practical Guide for Pastoral Care and Serious Mental Illness. They discuss the scope of the mental health crisis and how churches can respond in constructive ways.
Listen to this interview or continue reading.
Ann Michel: As a way of introducing the subject, could you begin by providing a general overview of the magnitude and scope of mental illness within American society today?
Matthew Stanford: We face a mental health disaster in our country today. It existed well before the pandemic, but the pandemic has only made things far, far worse. In any given year in the United States today, one in five adults and also one in five children and adolescents will suffer with a mental health problem. That’s an enormous number, probably close to 70 million individuals. Half of all chronic mental health conditions are in place by 14 years of age and 75 percent by 24 years of age. And probably the most disturbing statistic is that the majority of individuals — children and adults — with mental health problems will never receive any treatment.
These are serious and devastating conditions. We simply do not have a system that treats them adequately. For those who do receive treatment, the average period of time from the onset of symptoms to first treatment is 11 years. There’s no other medical condition where one would wait 11 years to initiate treatment. That means 11 years of trauma and devastation, relational problems, academic issues, employment issues. By the time a person receives treatment, if they ever receive treatment, they are carrying a lot of baggage that will be with them for the rest of their life. We can go on and on about the horror of the mental health care system and the people that suffer.
One bright spot is that people in psychological distress are more likely to engage a clergy before they engage a mental health care provider or physician. And that’s an incredible opportunity for the church to be a real front door in helping people get care.
But one bright spot is that people in psychological distress are more likely to engage a clergy before they engage a mental health care provider or physician. And that’s an incredible opportunity for the church to be a real front door in helping people get care.
Ann Michel: So congregations have a key role to play. And yet you say only a quarter of congregations have any kind of organized response or mental health ministry.
Matthew Stanford: Yes. It’s a little surprising. When I speak to pastors, they’re often very surprised to hear that they’re more likely to be engaged than physicians or mental health care providers. And some say, “Well, perhaps those are just people that aren’t as ill.” But research shows that those individuals engaging clergy for assistance are equivalently ill to those seeking out psychiatrists. They are people with very serious mental health care problems. But they don’t walk in and say, “I woke up today and I think I’m bipolar.” They say “I’m having spiritual problems. I’m having a relational problem. I’m having financial issues.” They talk about the same things as anybody else coming to a pastor for help. They just aren’t aware that a mental health problem is at the root of their problems. When you survey pastors, the vast majority, 70 to 80 percent say they don’t feel adequately trained to recognize a mental health condition in a congregant. Ninety percent of pastors provide some type of pastoral counseling, but then less than 10 percent ever make a referral. And less than a quarter of congregations ever develop any kind of structured approach to caring for or serving individuals with mental health problems. A large number of people are coming, but few are being served adequately. So it’s a real opportunity to serve people and help them get care. But it’s also an incredible ministry and evangelistic opportunity.
Data indicate that the people seeking assistance are not necessarily associated with the church. They may not even believe in God. Anyone in the general population struggling with these problems is more likely to engage a clergy first. So this is a real ministry opportunity as well as a service opportunity. It’s an opportunity to draw people into your fellowship and grow your church, to help your congregation learn to show grace and care, and to really help people that are suffering. And I think that’s really what God calls us to do.
This is a real opportunity to draw people into your fellowship and grow your church, to help your congregation learn to show grace and care, and to really help people that are suffering. And I think that’s really what God calls us to do.
Ann Michel: And it’s even more true in minority communities, that people are more likely to seek help from a church or clergy person than from a mental health professional, right?
Matthew Stanford: Yes, absolutely. In minority communities the church is still seen as more than just a place to go for spiritual involvement or comfort. It’s seen as a part of the broader community. So in minority communities, an even larger percentage of individuals will first seek assistance from churches. Here in Houston, where we train a lot of clergy and congregations, we’ve seen just an incredible response from the African-American and Hispanic community. Because they are even more greatly overwhelmed by these problems and not really equipped to deal with them.
Ann Michel. I think everyone is concerned about the pandemic’s impact on mental health. What are you seeing? And what should pastors and church leaders be looking for in this post-pandemic period?
Matthew Stanford: One of the first consequences we witnessed at our clinic, where we see people with serious mental illness, is that those who were doing well prior to the pandemic have struggled to maintain their stability. Because of the isolation, the disruption in schedules, and inability to access consumer goods and medications, people who were stable suddenly kind of decompensated and have really struggled through the pandemic. So pastors should have an eye out for any individuals with known mental health problems. They are likely to be the first ones suffering. And the goal is to try and help them get back to stability.
A second thing we’ve seen more generally is a dramatic increase in anxiety and depression with the disruptions, the changes in school and family dynamics, and concern for infection. Frankly, this is impacting just about everyone. Fifty percent of parents of teens are reporting worsened or new mental health care problems in their teenager since the beginning of the pandemic — mostly depression and anxiety. It’s worse in young women than it is in men. But it’s bad in men, as well. So pastors should watch out for really heightened depression and anxiety. But since the pandemic has gone on for so long, some people have probably figured out a way to kind of minimally cope with it. So they may not complain about depressive symptoms or anxiety. They may say “It’s hard for me to maintain a relationship. It’s hard for me to get up and get out. It’s hard for me to continue to do my job well.” Because this has been going on so long, they aren’t necessarily complaining that “I’m fearful” or “I’m sad.” But they’re struggling in daily activities as a result of a lot of depression and anxiety.
Every church doesn’t have to do everything. If we could just get every church to do something, it would make a difference.”
Ann Michel: You outline the four main components to a more holistic congregational approach to mental illness — what you call the “Four R’s.” Could you name them?
Matthew Stanford: We think of a mental-health-equipped church as one that can or does perform the “Four R’s.” First, they’re able to recognize when an individual is struggling with a mental health care problem. Second, they are able to make a professional referral and connect the individual to a mental health care provider. Third, they are trained to relate to individuals with mental health problems and/or their families in a compassionate and grace-filled way. And four, they have restorative programs that can meet the special needs and problems of individuals and families struggling with mental health problems.
Ann Michel: Mental health often seems like such a big and overwhelming problem, so I find stating those elements so clearly to be really helpful. Additionally, in your book you say churches that are engaged in prison ministries, recovery ministries, homeless ministry, or disaster response — these churches are already engaged in mental health ministry. They just don’t realize it. What general advice do you have for the many congregations involved in that kind of work?
Matthew Stanford: These types of ministries are very common and very important. I would also add to that list human trafficking ministries. But rarely do those ministries have a specific mental health component. Typically, they focus only on the spiritual aspect. That’s not a bad thing. But these ministries could be more effective with an added mental health component. That can be as easy as building relationships with local mental health care providers and working as a team. The church focuses on spiritual and personal growth and the mental health provider focuses on the mental health aspects. And they’re working as a team because ultimately the goal is an improved quality of life, which includes drawing closer to God and building up faith. Anything that we can do to help that individual move forward is really part of our ministry.
So often the modern church focuses merely on the spiritual. That’s our wheelhouse. And most of these ministries are built around the spiritual component. We share the gospel and provide discipling. But the church’s focus hasn’t always been that limited. If you look at the New Testament Church, they sold their goods and cared for one another’s physical needs, eating together and serving one another in a very physical, temporal way, in addition to their spiritual mission. I think we need to get back to that. We need to acknowledge that this person in front of me, this person that God’s brought to this ministry, has some physical needs. They have some mental needs. They have relational needs. And as a minister of reconciliation, a minister of the gospel, I have an opportunity not only to help them spiritually, but in these other ways as well. And, as out of my ministry to Christ, I’m able to improve their life spiritually and in a temporal sense. Because God created us as both spiritual and physical beings.
A church is a wonderful place for that recovery to occur. Because, again, we have a hope that transcends circumstances, which is not something that the world has to offer. We have a foundation for recovery that is unchangeable and absolute.
Ann Michel: So a more holistic mindset is required to meet all of a person’s needs. You make a strong case for educating and equipping clergy to recognize and respond to different types of mental illness. But what can a congregation do to equip other frontline leaders? I’m thinking of staff, small group leaders, youth workers, mission workers who are so often the face of the church as it engages others.
Matthew Stanford: A congregation needs to equip itself before people show up. You have to do your due diligence before someone is standing in front of you needing assistance. But I don’t think everyone has to be trained at the same level. If the clergy, the ministry staff, lay ministry leaders and volunteers are trained to recognize mental health issues, that a good foundation. Not everyone needs to be able to make referrals. But everyone needs to be able to recognize if an individual’s problems are more than spiritual and may require mental health care. Then some people, maybe some ministry staff, are trained as point persons to conduct an assessment, make a referral, follow up, and make sure the person is connected with the right ministries, say a support group. So, it is a stairstep approach. At one level, everybody can recognize mental health care problems. And then they move the individual on to more specialized ministries and trained individuals within the church. And ultimately, it allows the person to access some level of therapeutic support for free. Because mental health care is extremely expensive, finances are a huge barrier to people getting to care. So if a church can provide that kind of support and ongoing care, the person only has to access maybe one mental health care provider. And that really takes a burden off of them as well.
Ann Michel: So what first steps can a congregation take if it’s just beginning to think about this issue — to help destigmatize mental illness, begin the process of educating the congregation, and have a more open conversation?
Matthew Stanford: It’s a conversation. And it’s really up to the leadership of a church to start that conversation. Undoubtedly, there are people in the church who want to have the conversation, but the leaders are the ones who can get it off the ground. So, I recommend perhaps a sermon series on mental health issues or on particular biblical characters that struggled with mental health. David is a great one if you want an easy, easy one. The vast majority of his psalms are songs of lament as he struggles with his depression.
Not everyone needs to be able to make referrals. But everyone needs to be able to recognize if an individual’s problems are more than spiritual and may require mental health care.
It’s also important to communicate the touch points within the church. Do you have support groups? Are you talking about the support groups? Have you had someone give a testimony of how the support groups have been effective and helpful for them? Do you have specialized ministries like addiction ministries and homeless ministries? Are you communicating to the church that those exist, how people get into those programs, how they work? Again, testimonies are always very important. So, often, there is often a breakdown in communication. A churches may actually have referral lists and opportunities for referral, but they simply never communicate it to the church. They wait until somebody comes in and asks for that. So, it’s very important to communicate from the start. Sunday school classes or Bible studies that focus on mental health for a certain season can be an opportunity for those struggling with real problems and those just interested in knowing more. I love pastoral care teams who can walk alongside individuals with mental health concerns, offering a listening ear and just being there for support. I think these are all ways to get the conversation going. But also, bring in mental health care providers to do trainings or workshops. Every church could benefit from having a mental health care provider come in and do a one-time training on suicide prevention. No one really gets upset about that. No one wants anyone to die by suicide, so it’s a great way to begin to get your congregation equipped.
Ann Michel: Your book profiles a number of different congregations. Many are larger churches. But I was surprised to see a few that are smaller. Since we all know that the vast, vast majority of congregations in the US are small membership churches, can you address mental health ministry in small or rural church contexts?
Matthew Stanford: Most churches in the United States are 75 or less. They may think they don’t have the resources or the human capital or the ability to start any kind of mental health ministry. But absolutely they do. I’ll give you an example of probably the smallest church where we’ve ever done training. It’s a church that literally worships 15 on Sunday morning. They have a bi-vocational pastor who works full time at another job. They don’t have a lot of people to volunteer. And they have very limited physical resources. And so we trained a subset of people — mostly women that oversee a lot of their ministries — to recognize mental health care problems. And we provided them with cards for a mental health referral line. If someone calls that line and explains their problem, clinicians will help them find a mental health care provider in the community. So even in this small church with very few resources, they have people who can recognize mental health care problems and provide a phone number that a person can call to get a referral. It’s that simple.
In a larger church, you might have a lot of trained staff. You might have specialized ministries. But really, it’s all about getting people to the same starting point. One church we profiled was in a very rural area that has virtually no mental health care providers. Yet they saw tremendous need through probation and parole in their county. And so they partnered with probation and parole and offer some support groups and some mentoring. It’s a tremendous benefit to the community in that county. So it’s really about assessing the needs of your area and how you want to help. I often say, “Every church doesn’t have to do everything. If we could just get every church to do something, it would make a difference.”
Most churches in the United States are 75 or less. They may think they don’t have the resources or the human capital or the ability to start any kind of mental health ministry. But absolutely they do.
Ann Michel: Your book is so very practical and provides really clear information and recommendations. But it also addresses the spiritual component of ministering to those with mental illness. Could you speak a word of hope or reassurance to listeners who may be struggling with mental illness themselves or within their family or their church community? Just what does our faith say to them?
Matthew Stanford: Absolutely! If you are struggling with a mental health care problem or your loved one is struggling, there absolutely is hope. I’m not sure how much more your mental health problem can be minimized or your symptoms relieved. But there’s a hope that transcends circumstances. And that’s Jesus Christ. And this is a faith of transformation. God is changing us every day into the likeness of his son as we submit to his indwelling Spirit. And you can always grow in your faith regardless of your symptoms. Your relationships can be better tomorrow than they are today. Your symptoms can be better tomorrow than they are today. Recovery is a process just like sanctification is a process. I see the recovery process very much like our own spiritual transformation. We have the salvation experience that’s one and done, but we have the sanctification process. And recovery is much the same way. And a church is a wonderful place for that recovery to occur. Because, again, we have a hope that transcends circumstances, which is not something that the world has to offer. We have a foundation for recovery that is unchangeable and absolute. And on those bad days when circumstances are overwhelming, we still have a Savior that overcame the world and dwells in us. And so we have something to hold on to that really can never be taken away from us.
 Related Resources
Related Resources
- Madness and Grace: A Practical Guide for Pastoral Care and Serious Mental Illness (Templeton Press, 2021) by Dr. Matthew Stanford, available at Templeton Press and Amazon
- “Pastoral Care in the Coronavirus Crisis,” a Leading Ideas Talks podcast episode featuring Michael Koppel
- “Tackling Tough Topics in Church,” a Leading Ideas Talks podcast episode featuring Elizabeth Hagan
- Ministry with Veterans by Jane Donovan
- Leading a Ministry with Homeless People by Rudy Rasmus